Forgot your password?
An introduction to CTO for fellows
Dr Edwina McNaughton, Complex Intervention Fellow
Chronic total occlusion (CTO) PCI has become more widely practiced in the last decade. With the advancement of technology, skills and training, the success of CTO PCI has increased in recent years. The ESC in 2018 gave a Class 2A recommendation for CTO PCI.1 Despite this, there has been reluctance to treat CTO’s due to a lack of survival benefit. Of patients with ischaemic heart disease, 25% have a CTO. Only 9% of these are attempted to be recanalized.2 The CONSISTENT CTO trial showed that out of 230 patients, 90% of CTO’s were opened successfully by interventionists with expertise in CTO.3
Although there have been no studies proving survival benefit, some studies suggest that quality of life and angina burden/frequency is reduced as reported by patients. The EURO-CTO trial demonstrated an improvement in quality of life and symptom management following recanalization of CTO at twelve months using Seattle Angina Questionnaire and European Quality of Life–5 Dimensions assessment.4 The IMPACTOR-CTO trial showed the importance of re-canalization of the RCA in improving functional status and quality of life, without impact on clinical outcomes.5 The DECISION-CTO trial did not see any reduction in major adverse cardiac event (MACE) rates at four years for patients treated with PCI versus those managed medically, although 20% crossover was noted into the PCI arm. However, it did highlight low complication rates during CTO angioplasty.6
Interestingly, the Syntax trial 10 year outcomes demonstrated that if patients are left with incomplete revascularization, the risk of all-cause mortality is higher at SYNTAX score >8 (50%) compared to SYNTAX score 0-4 (24%).7
Ultimately patient selection is important. Those who have a significant angina burden or significant impact on quality of life may benefit most. CTO PCI carries a slightly increased risk of adverse outcomes given the procedural complexity. With appropriate training, we should be well equipped to treat these rather than manage medically.
Procedure preparation
Ensuring the team are adequately trained is important to aid the likelihood of success. Ensuring appropriate CTO kit is available in the cardiac catheter lab is essential prior to commencing a procedure.
Access and angiographic assessment
CTO PCI generally should be performed as an elective procedure, with planning prior to the procedure to maximise success and minimise contrast and radiation use. Dual access is important to fully understand the CTO and visualise the strategic options available to attempt CTO PCI. Bi-radial access in the first instance is adequate; most CTO cases can be completed with 7 French guide catheter. A passively supportive guide catheter is important, typically Voda Left, XB or EBU catheters for the left coronary artery, and AL or 3D curves for the right coronary artery. The use of guide extension catheters may also be required to overcome poor support.
The use of road-mapping angiographic views at the start of the procedure is crucial. Views which are useful include:
Right Coronary Artery
Left Anterior Descending Artery
Left Circumflex Artery
A donor guide, a guide engaged in the contralateral coronary system to aid visualisation, should have a workhorse wire routinely placed in the donor vessel. This maintains catheter position, allows easy engagement and disengagement and also importantly expedites any treatment of donor vessel injury, which can cause rapid deterioration in the context of a contralateral CTO.
The use of intravascular imaging is important to aid successful outcomes and also to reduce contrast use.
It is important to understand there are many methods to crossing an occlusive lesion. Wire escalation methods can be anterograde or retrograde (AWE/RWE). This entails changing your wire selection based on the characteristics you encounter and need to overcome. Dissection reentry techniques again can be used either anterogradely or retrogradely (ADR/RDR), these involve dissecting sub-intimally into the vessel architecture past the occlusion, with re-entry into the true vessel lumen below the occlusion.
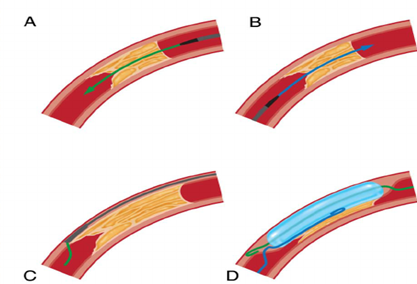
Figure 3: CTO strategies A) Anterograde wire escalation, B) Retrograde wire escalation, C)Anterograde dissection re-entry, D) Retrograde dissection re-entry (Image reproduced from A guide to mastering Anterograde CTO PCI)
CTO body, distal cap and landing zone
The length of the CTO lesion as it increases (>20mm) makes intimal wiring less likely and increases procedural time. A heavy burden of calcification and vessel tortuosity are other features which may influence initial strategy away from AWE.
The vessel beyond the distal cap and before the origin of a major side-branch is known as the distal landing zone. If there is a bifurcation near to the landing zone, it may deter operators from an anterograde dissection re-entry approach as this may result in loss of the side-branch patency.
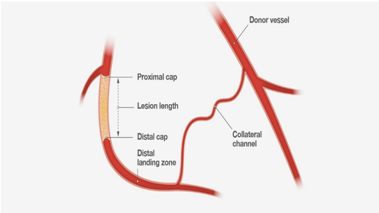
Figure 1: Understanding the varying parts of a chronic total occlusion are important for successful outcomes (Image reproduced from A guide to mastering Anterograde CTO PCI)
Collateral channels facilitate visualisation of the distal target. It is important to understand the origin and course of the collateral vessel and whether it is useful as an ‘interventional’ collateral if considering a retrograde approach. Typically septal collateral channels are preferred as the risks of complications such as tamponade are limited.
J-CTO score
The Japanese CTO score was developed to assess probability of a successful CTO procedure. The five main components are:
Scores in the lower range suggest a straightforward CTO, higher scores reflect more complex lesions.
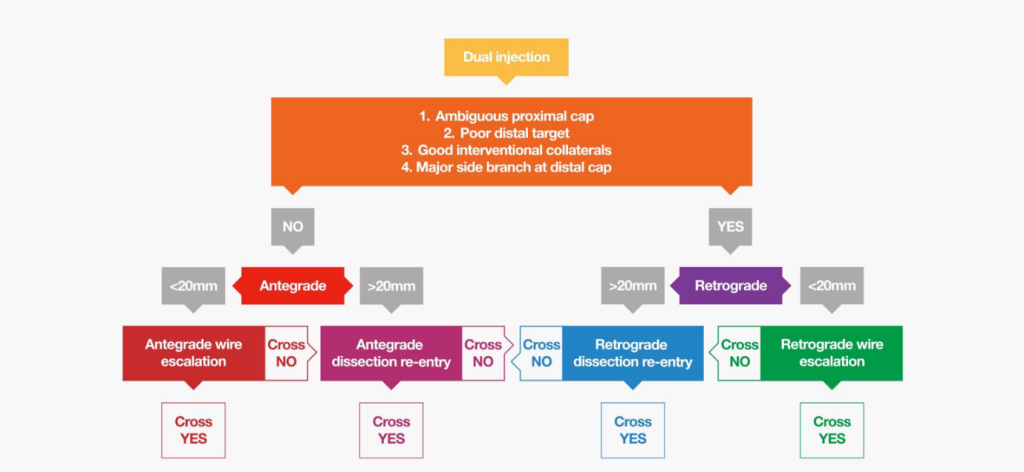
Figure 2: The hybrid algorithm (Image reproduced from A guide to mastering Anterograde CTO PCI)
The hybrid algorithm
There are four angiographic anatomical features that influence initial strategy when using the hybrid algorithm:
Wire selection
Wire selection should be based on their properties and the lesion characteristics you need to overcome. The use of a microcatheter is recommended to further enhance the wire’s properties and to aid wire exchange. Trapping balloons are also useful for switching out equipment. Below is a useful table of wires commonly used in CTO intervention8.

Table 1: Commonly used guidewires for CTO intervention8
Intravascular imaging
Intravascular imaging is invaluable in CTO procedures. IVUS is preferred due to OCT needing high pressure contrast injection, which can propagate dissection. IVUS can aid in identifying pathology, confirming true lumen position, and planning stent size, length and expansion targets. It can also aid optimisation of apposition of implanted stents for more durable results from CTO PCI.
Ultimately, CTO PCI success is achievable if the operator has selected appropriate patients, assessed the lesion adequately and prepared a strategy prior to intervention. With appropriate training, these lesions can be treated and patient quality of life improved.
References